Human Sperm Assay (HSA)
A detailed assessment of sperm health to diagnose male fertility issues
What is Human Sperm Assay (HSA)?
The Human Sperm Assay (HSA) is a specialized test used to analyze sperm health and function. Unlike a standard semen analysis that primarily checks sperm count, motility, and morphology, HSA provides a more in-depth evaluation of sperm quality, including its ability to fertilize an egg. This test is crucial for identifying underlying causes of male infertility and determining the best course of treatment for conception.
Why is HSA Important for Assessing Male Fertility?
HSA plays a vital role in diagnosing male fertility issues, particularly conditions like Azoospermia, Asthenozoospermia, and Teratozoospermia, which can significantly impact a man’s ability to father a child.
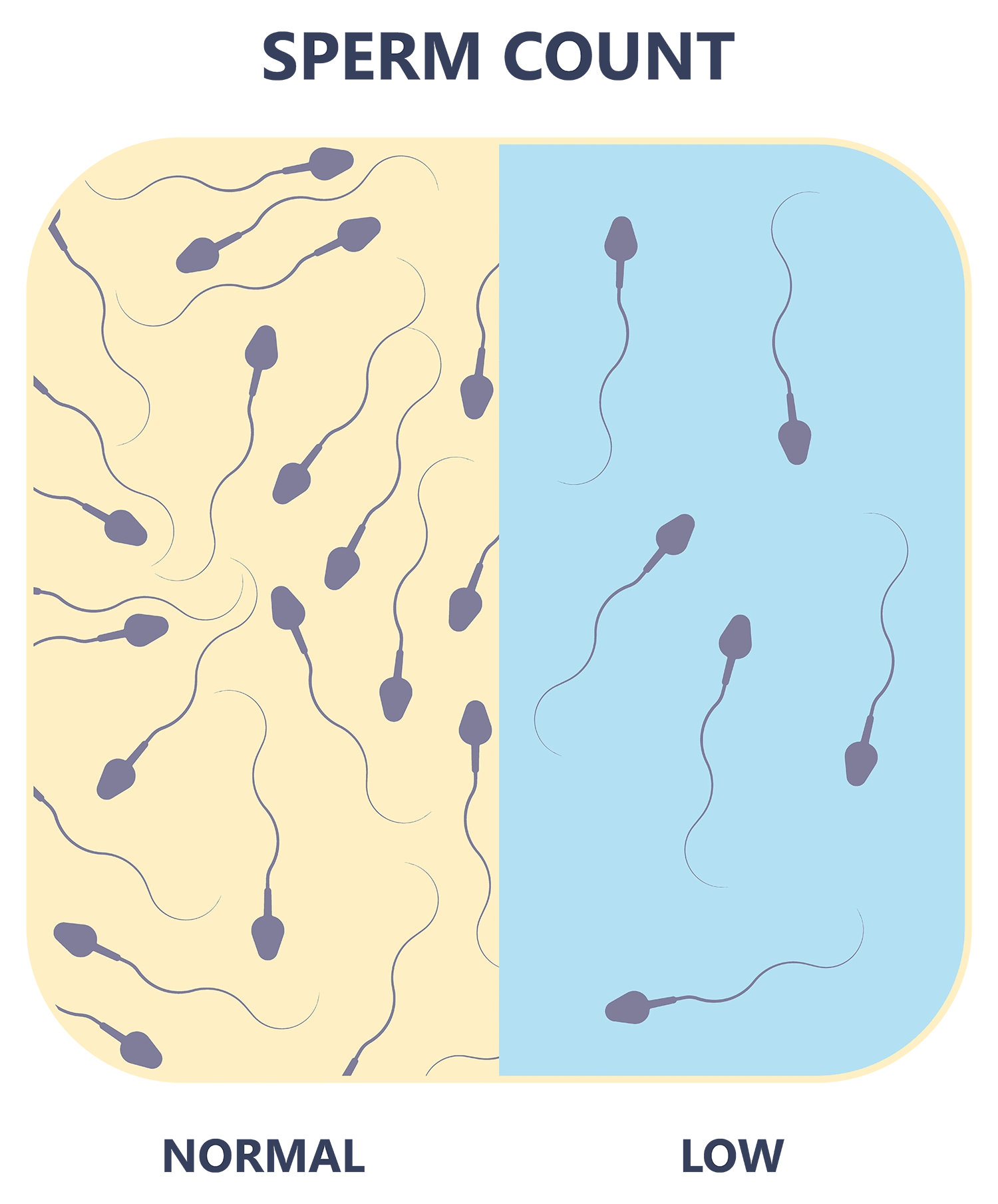
Azoospermia - Absence of Sperm
Azoospermia is a condition where no sperm is present in the ejaculate. This can be caused by:
- Obstructive Azoospermia – Blockages in the reproductive tract preventing sperm from mixing with semen.
- Non-Obstructive Azoospermia – The testicles do not produce enough or any sperm due to hormonal imbalances, genetic conditions, or testicular failure.
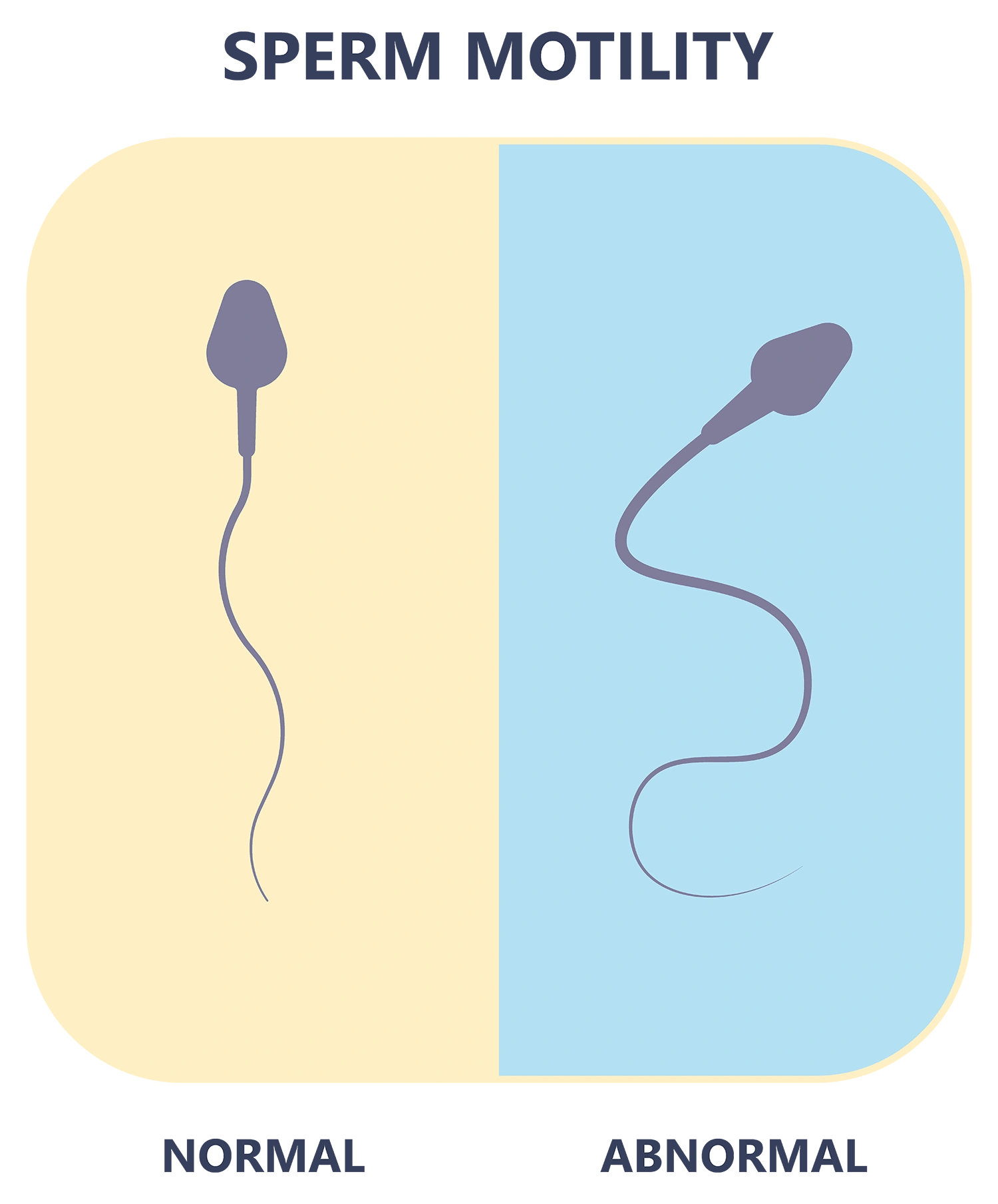
Asthenozoospermia - Low Sperm Motility
This condition is characterized by poor sperm movement, reducing its ability to reach and fertilize an egg. Common causes include:
- Lifestyle factors (smoking, alcohol, poor diet)
- Infections or inflammation of the reproductive system
- Hormonal imbalances
- Genetic factors
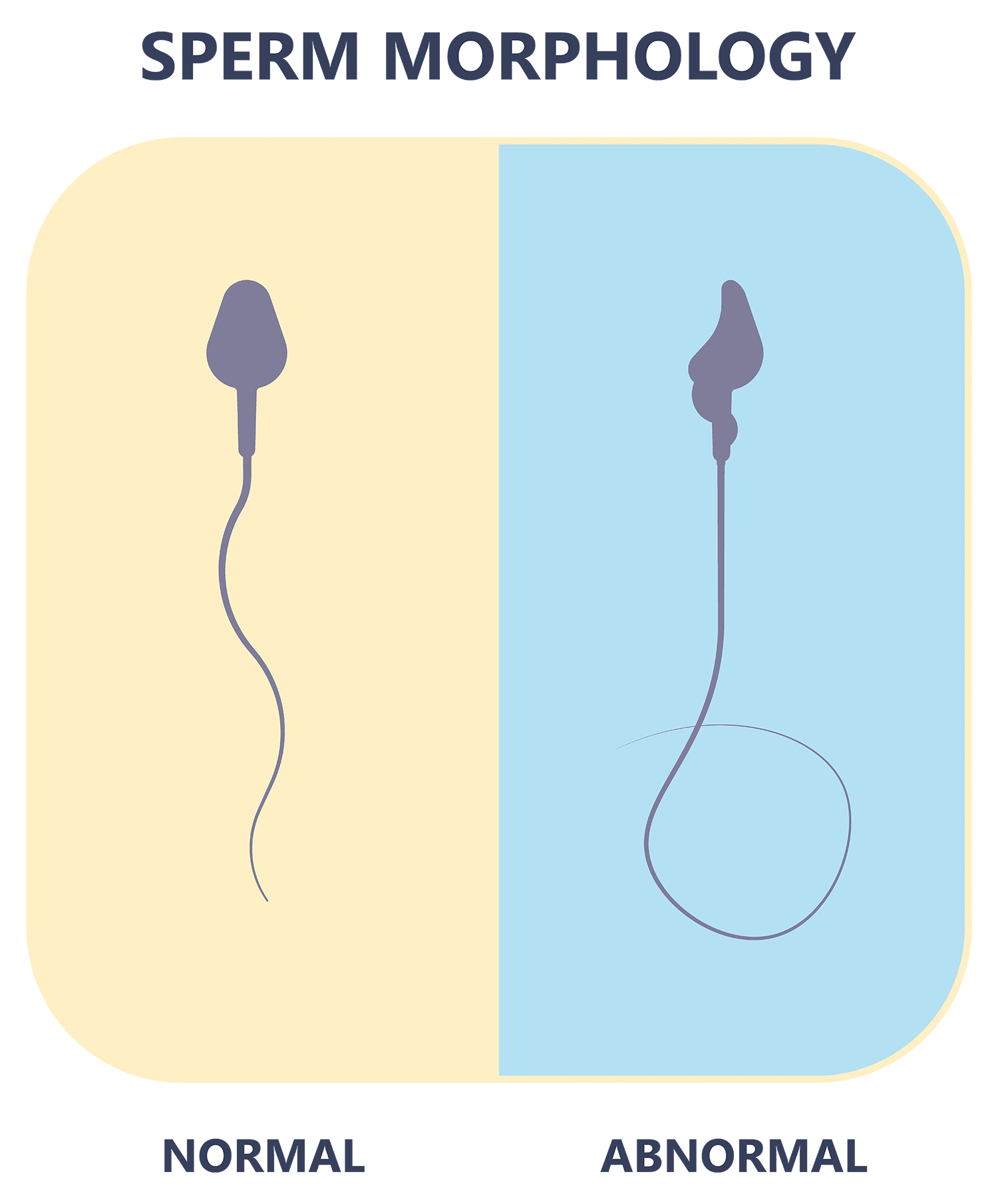
Teratozoospermia - Abnormal Sperm Shape
Teratozoospermia refers to an increased percentage of abnormally shaped sperm, which may affect their ability to fertilize an egg. Possible causes include:
- Genetic disorders
- Exposure to environmental toxins
- Varicocele (enlarged veins in the scrotum)
- Testicular injury or infections
HSA plays a vital role in diagnosing male fertility issues, particularly conditions like Azoospermia, Asthenozoospermia, and Teratozoospermia, which can significantly impact a man’s ability to father a child.
Treatment Options for Azoospermia, Asthenozoospermia & Teratozoospermia
Depending on the severity and cause, these conditions can be managed through medical or surgical interventions.
Hormonal Therapy
Used to correct hormone imbalances affecting sperm production.
Lifestyle Modifications
Improving diet, quitting smoking, reducing alcohol intake, and managing stress can enhance sperm health.
Antibiotic or Anti-inflammatory Treatment
Helps resolve infections that may be impairing sperm production or motility.
Varicocele Repair Surgery
Can improve sperm quality by restoring normal blood flow to the testicles.
For Obstructive Azoospermia, surgical sperm retrieval techniques like PESA, TESA, or Micro TESE may be performed to extract viable sperm directly from the testes.
Whether you are facing one or multiple challenges, Bud IVF is here to guide you with personalized care and expert solutions tailored to your unique needs.
Fertility Options When Treatment is Not Effective
If natural conception is not possible, assisted reproductive technologies (ART) offer hope:
If sperm motility is slightly impaired but still viable, it can be directly placed inside the uterus to enhance fertilization chances.
Recommended for cases where sperm abnormalities affect natural conception. Eggs are fertilized outside the body, and healthy embryos are implanted in the uterus.
Specifically designed for severe male infertility cases, where a single healthy sperm is injected directly into the egg. Donor Sperm – In cases where sperm retrieval is unsuccessful or quality is too poor, using donor sperm may be an option.
In cases where sperm retrieval is unsuccessful or quality is too poor, using donor sperm may be an option.
FAQs
How is HSA different from a regular semen analysis?
HSA provides a more detailed assessment of sperm function and fertilization potential, whereas a standard semen analysis mainly checks sperm count, motility, and morphology.
Can lifestyle changes improve Azoospermia, Asthenozoospermia, or Teratozoospermia?
Yes, adopting a healthy diet, quitting smoking, reducing alcohol intake, and maintaining a healthy weight can significantly improve sperm quality.
Is Azoospermia treatable?
It depends on the cause. If due to a blockage (Obstructive Azoospermia), surgery may restore sperm flow. If due to testicular failure (Non-Obstructive Azoospermia), hormonal therapy or sperm retrieval techniques may be considered.
What is the success rate of IVF/ICSI for male infertility?
Success rates vary depending on individual cases, but ICSI offers high success rates by injecting a single viable sperm directly into the egg, making it an effective treatment for severe male infertility.
How can I get tested for male infertility?
A fertility specialist will recommend tests such as semen analysis, hormone testing, and HSA to diagnose sperm-related issues. Scheduling a consultation is the first step toward identifying and addressing fertility concerns.
